DIABETIC RETINOPATHY
Structure of the Eye
The inner most layer of the eye is composed of delicate tissue called the ‘retina’ which is comparable to the film inside a camera. Visual impulses are received by specialised cells in the retina and transmitted to the brain via the optic nerve. The central part of the retina which is the most sensitive and enables us to see clearly is called the ‘macula’.
DIABETIC RETINOPATHY is the term applied to specific changes in the retina which can occur in people with diabetes mellitus. The incidence of retinopathy seems to be directly related to the duration of diabetes rather than to its severity or control.
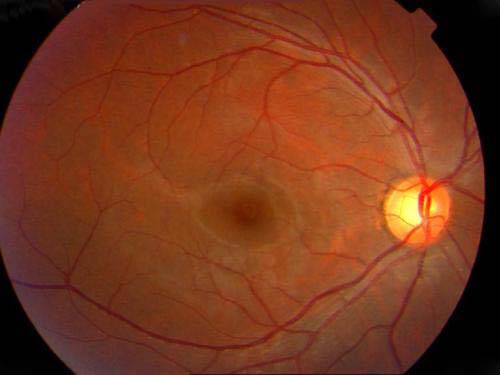
The changes involve the small blood vessels of the retina. The inner lining of these blood vessels is weakened and small out-pouchings occur. These are called ‘micro-aneurysms’. The blood vessels also become abnormally permeable and allow substances to leak freely into spaces where they should not normally enter. This results in water-logging of the retina called ‘edema’ and deposition of lipid material in the retina called ‘exudates’. These changes cause symptoms of blurred vision if situated at the macula. This stage of the disease is called BACKGROUND or NON-PROLIFERATIVE DIABETIC RETINOPATHY, as seen in picture above.
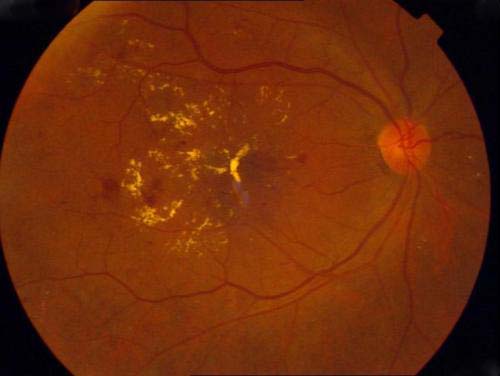
The more serious change in diabetic retinopathy is the closure of retinal capillaries. This causes a deficiency of oxygen to the retinal tissues resulting in the growth of abnormal new blood vessels on the retina (as seen in the pictures below). These new vessels are weak-walled with a tendency to readily bleed into the eye leading to sudden and profound visual loss. Seeing black spots or floating objects of various shapes or cob-web like shapes are usually an indication that a bleed has occurred. This bleed is called ‘vitreous haemorrhage’.


This stage of the disease is called ‘PROLIFERATIVE DIABETIC RETINOPATHY’. If the bleed is massive then vision is lost or blurred completely. Such bleeds may clear spontaneously or may remain as such. Sometimes repeated bleeds can occur leading to the formation of fibrous tissue which by pulling on the retina, causes ‘retinal detachment’, a serious condition needing surgery for its management.
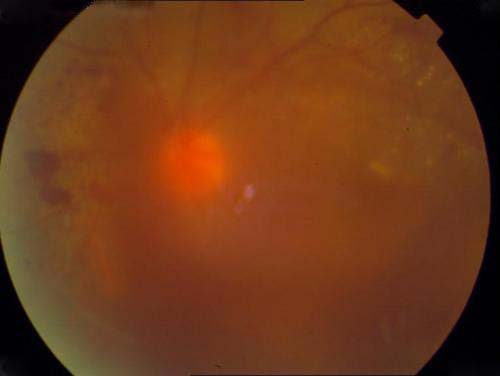
Note the severe haze due to which the retinal details cannot be seen.
An eye with marked changes of diabetic retinopathy may have good vision and be totally symptom-less as long as the macula is left unaffected. A reduction in vision occurs if the macula becomes waterlogged, becomes involved ina retinal detachment or if the vitreous haemorrage covers it up.
What Are The Symptoms Of Diabetic Retinopathy?
As mentioned above the patient may be having severe retinopathy but symptoms may be absent because the macula is unaffected. That is why all diabetes, especially those who have diabetes for more than 5 years, should get their eyes examined every year by an eye surgeon who is specially trained in the management of retinal diseases. If detected at the right time then treatment with LASER photocoagulation can in most cases delay the sight threatening effects of diabetic retinopathy for a considerable period of time.
How Is Diabetic Retinopathy Treated?
While good control of diabetes is important in delaying the involvement of the retina due to diabetes, but being a progressive and incurable disease it ultimately does lead to retinopathy at some stage of the patient’s life. No medicine has yet been found to have any effect on the progress or prevention of diabetic retinopathy. Meticulously planned and executed multi-centric studies in the USA have proven without doubt the efficacy of LASER PHOTOCOAGULATION in the treatment of early and advanced diabetic retinopathy. LASER photocoagulation has thus become the mainstay of treatment of diabetic retinopathy the world over with medicines having only a supportive role to play.
Medical treatment usually consists of Injections of certain medications into the eye to reduce the ‘edema’ or the water-logging of the retina to facilitate the effective use of LASER photocoagulation. Another type of injection that has been found to be useful is called ‘Anti VEG-F’ and this helps to prepare the eye for surgery, making it somewhat less complex and hazardous. Thus it is usually given 10-15 days prior to surgery for diabetic retinopathy.
What Is Fundus Fluorescein Angiography – FFA Test?
This is a special test wherein a dye called ‘fluorescein’ is injected into the patient’s blood stream and once the dye reaches the retina pictures are taken of the retina using a special camera called ‘fundus camera’. This test has to be done in all patients undergoing laser treatment as it shows the doctor exactly what is the severity of the retinopathy. Also, when the test is repeated after laser treatment has been completed the effectiveness of the treatment can be evaluated and the film can be kept as a permanent record for future reference. All patients with significant retinopathy must periodically undergo this test.
The white patches seen in the picture below are the area of the leaking blood vessels as seen on fluorescein antiography.
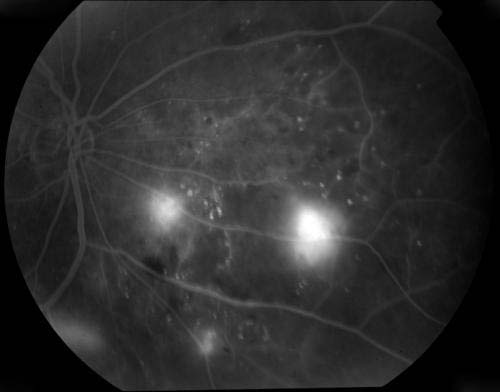
For this test the patient should be fasting for 3 hours and should be accompanied by an adult. There is no discomfort during this test except for the needle prick when the dye is injected and the dazzling effect of the camera flash. For about 2-3 days after the test the patient passes greenish yellow urine which should be ignored. For 3 days after the test the patient should not get his blood sugar tested as the result can be erroneous due to interference from the dye which is circulating in the body. A few people experience nausea during the test, but it passes of rapidly. A very small percentage of patients may be allergic to the dye and may experience varying degrees of reaction from itching to severe difficulty in breathing, but such cases are extremely rare and can be easily treated. Serious life threatening reactions are exceptionally rare, but can however occur. On the whole this is a very safe test having hardly any side effects.
What is LASER Photocoagulation?
LASER is a type of highly focused and concentrated light (green in colour for the treatment of retinopathy) that is produced inside a special and expensive machine called the ARGON LASER. This light has the power to coagulate living tissue of certain type that is present in the retina of the eye. This light is focused on to specific parts of the retina by the doctor to selectively destroy those areas. This is very similar to the manner in which paper gets burned when sun light is properly focused on it using a lens.
How Does Argon Laser Photocoagulation Help?
The areas that are selectively treated with the laser are those which have the edema, the microaneurysms and the leaky, newly formed blood vessels that have a tendency to bleed and cause vitreous haemorrhage. Thus the main purpose of treatment is to arrest the progress of the disease at the stage at which it has been detected thereby preventing or delaying certain vision threatening complications that may ensue later. Photocoagulation does not necessarily make the patient see better or feel better although in some limited conditions the vision may improve. It does not eliminate the black spots or ‘floaters’ that the patient may be seeing and it does not resolve the vitreous haemorrhage if it has already occurred. In some instances where the disease is progressing very rapidly photocoagulation may not have any effect at all on the retinopathy. It takes about 6-8 weeks for the effect of photocoagulation to come. During this period there is always the risk of bleeding from already existing new blood vessels. Once the desired effect is obtained these new blood vessels usually regress and are no more a threat unless they crop up from some other area of the retina.
Without photocoagulation, however, there is much higher risk of progress of retinopathy with the associated visual loss. Thus the risks of photocoagulation are much lesser as compared to the risk of progressive diabetic retinopathy.
How Many Times Will Photocoagulation Be Needed?
If the patient has early retinopathy with only macula involvement leading to blurring of vision then usually only one sitting of treatment with the laser is needed. The patient is again seen after 6 – 8 weeks and if residual edema is still present then one more sitting may be advised.
Patients having more advanced disease in the form of proliferative retinopathy generally require between 1 to 5 sittings depending on the severity of the condition. These sittings are done on successive days or with an interval of one week between sittings.
Patients who were earlier treated with one sitting for macular edema may later develop proliferative retinopathy and will require more sittings according to the severity of retinopathy.
What Are the Side Effects of Laser Treatment?
There are hardly any side effects. The vision is quite blurred immediately after treatment specially if the macula has been treated but it clears up in a few hours. The patient should not move his eye during the treatment session and should keep looking in the direction he is asked to by the doctor or it will be difficult to focus the laser beam at the proper area.
In a few cases the vision may continue to deteriorate despite photocoagulation. This is due to the nature of the disease and un-preventable changes that may take place at the macula.
What Precautions Have to be Taken after Laser Treatment ?
No special precautions have to be taken during or after laser treatment. The treatment is done on out-patient basis and each session lasts 15 to 20 minutes only. The patient has to continue his diabetic medication and blood pressure medicines, if any and diet. In case he has proliferative disease then he should avoid strenuous exercises and running as jerks to the head can cause bleeding from the new vessels. Apart from this no other precautions are required.
The patient has to be constantly under the supervision of his eye doctor and must come for regular check-ups which are generally every 3 to 6 months. During these visits the FFA may have to be repeated and more laser treatment may be needed. He should also keep his diabetes under control and take treatment of other problems like blood pressure, kidney problem and heart problem if any.
What if the Retinopathy Progresses Despite Laser Treatment?
As mentioned earlier diabetes is a progressive, incurable disease. By treating the retinopathy with laser we can delay sight threatening complications that occur. We cannot reverse the course of the disease or cure it. At best the disease may stabilise and become stationary, but in some cases it continues to progress relentlessly till ultimately there is massive vitreous haemorrhage and other sequelae, but this is generally a slow process if the diabetes and other parameters are well controlled . In some cases more laser can be done while in others ‘cryotherapy’, which is a type of cold fomentation helps.
What Is Vitrectomy and When Is it Required?
If the vitreous haemorrhage does not spontaneously resolve or if the retinal detachment involves or threatens the macula then surgery is the only choice. This surgery requires expensive equipment, instruments and surgical skill. It is done only at a few specialised retinal centres in India including Mansarovar. It is called ‘vitrectomy’. It involves entering the eye and physically removing the blood and abnormal blood vessels and fibrous membranes from the retinal surface. We, at this hospital are doing this surgery in selected cases after a thorough evaluation of the eye. The patient has to understand that this is a very complicated surgery and the results may not always match the expectations of the patients, but the vision generally improves with time after the surgery if other parameters like blood sugar, lipid profile, renal functions are kept under control.
For comments and questions, click here.